CATEGORY: Health Informatics Journal
SOURCE: Sage Journals, October 15, 2025, https://doi.org/10.1177/14604582251387969
Advanced monitoring, alerting and feedback in early risk mitigation for pancreatic cancer
George Manias1,2, Nelina Angelova3, Diana Kirova4, Aristodemos Pnevmatikakis3, Pencho Stefanov4, Fabio Melillo5, Oscar Garcia Perales6, Konstantina Kostopoulou3, Sofoklis Kyriazakos3, Dimosthenis Kyriazis1
1Department of Digital Systems, University of Piraeus, Pireas, Greece
2Jheronimus Academy of Data Science, Tilburg University, Tilburg, Netherlands
3Innovation Sprint, Brussels, Belgium
4Strypes ICT, Sofia, Bulgaria
5Engineering Ingegneria Informatica SpA, Rome, Italy
6Information Catalyst, SL, X`ativa, Spain
Abstract
A novel patient monitoring system is introduced, designed to support early risk mitigation in pancreatic cancer through personalized health interventions. The system aims to strengthen patient engagement and proactive care by enabling healthcare practitioners (HCP) to assign dynamic, data-driven and personalized mitigation plans. Central to this system is a user interface that allows HCP to review and assign tailored mitigation plans to patients. These plans are formulated based on primary clinical data and enriched with secondary behavioral data, such as wearable-derived metrics and self-reported inputs. These inputs are continuously collected, transformed into Holistic Health Records (HHRs), and stored in a scalable platform for integration with ML-based trend analysis and visualization. The article outlines the system’s technical architecture, patient data evaluation logic, and user experience across both the HCP interface and patient app. Evaluation by end users via questionnaires demonstrated improved adherence to plans and higher-quality behavioral data. This monitoring platform offers a promising tool for facilitating early risk intervention in pancreatic cancer care. By integrating multi-source patient data into actionable strategies and fostering bidirectional engagement, it bridges the gap between clinical insight and patient participation, contributing to holistic health management.
Introduction
The integration of internet and technology into healthcare has opened new horizons for patient care and disease management, marking a significant shift from traditional methods to more personalized and proactive approaches.
1–3 The iHelp platform
4 is one such comprehensive solution designed to augment the capabilities of HCPs across various domains of patient management. This innovative system consolidates multiple components to offer a range of functionalities aimed at enhancing patient care, predicting health outcomes, and promoting healthier lifestyles. The patient Monitoring, Alerting and Feedback (MA&F) subsystem is the part of the iHelp platform that tailors and delivers the treatment plans.
To arrive at this point though, iHelp involves a data collection and processing subsystem
5 that provides the patient MA&F subsystem with the patient context, as it is mapped into proprietary Holistic Health Records (HHRs) stored in the BDP.
6 The HHR data is analyzed towards early risk predictions and personalized prevention measures.
7,8Both raw and processed data is visualized in the Decision Support System (DSS) at the core of the iHelp platform. DSS is designed to support the dynamic needs of healthcare professionals and their patients. It acts as a central hub, providing seamless access to the platform’s diverse functionalities. HCPs can efficiently manage patient information, access predictive analytics, and implement personalized care plans without navigating through multiple applications or interfaces. Via DSS, the iHelp platform empowers HCPs to make informed decisions, tailor treatment plans, and manage potential risks more effectively.
Mitigation and action plans form the backbone of this patient care delivery and focus on promoting a healthier lifestyle and behavioral change in patients, while also tackling known comorbidities of the disease. Recognizing the impact of lifestyle choices on overall health, and the impact digital therapeutics have in managing, preventing and treating various conditions in the modern world,
1–3 the MA&F subsystem of iHelp enables the assignment of customized action plans. These plans are designed to encourage positive health behaviors and are delivered through Healthentia,
9–12 a patient companion app and its associated supporting backend services. The data collected and visualized through the Healthentia app includes both real world data (RWD) measurements (from integrated IoT devices like activity trackers) and self-reports (questionnaires, manual input records). Observed fluctuations on the latest data entries connected to an action plan shape future personalized care giving. Care delivery is also done via the Healthentia mobile app, namely its virtual coach
9 that delivers dialogues to the patients. These dialogues offer continuous support and motivation, information on achievement or failure for the past period’s actions, and educational content. All dialogues are curated by experts and are triggered by the MA&F subsystem of iHelp and the supervision of the HCPs. This aspect of the iHelp system is instrumental in engaging patients in their own health management, fostering adherence to health recommendations, and ultimately leading to improved health outcomes.
The integration of these diverse functionalities within a single DSS represents a significant advancement in healthcare technology. The iHelp platform exemplifies how digital solutions can transform patient care, offering a more personalized, predictive, and participatory approach to healthcare. By equipping HCPs with the tools to remotely manage their patients and promote healthier lifestyles, the iHelp platform addresses the multifaceted nature of patient care in the digital age. This introduction sets the stage for a detailed exploration of the iHelp platform’s monitoring, alerting and feedback components, showcasing their operation and impact on healthcare delivery.
Methodology
The MA&F subsystem is used in different studies of iHelp related to pancreatic cancer. The studies have diverse aims falling into two groups: (i) individuals that are coached into healthier lifestyles to reduce their risk, and (ii) patients that are coached towards improved quality of life.
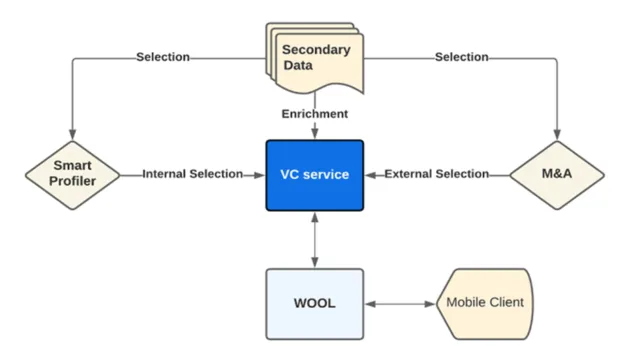
The MA&F subsystem functionality is delivered by four components. Two of them, the Monitoring & Alerting and the impact evaluator components are located in the iHelp BDP. The other two, the Smart Profiler and Virtual Coach components are part of Healthentia and are utilized by iHelp. The Monitoring & Alerting component is the starting point, as it manages the personalized care plans. Then, the Smart Profiler understands the patient context and the Virtual Coach handles the interaction of the patient with the delivered content. Finally, the Impact Evaluator understands the effect of the content delivered to the patient. These components are detailed in the following sub-sections.
Monitoring and alerting
The Monitoring and Alerting component facilitates the management and improvement of patient health through personalized action plans, leveraging both primary and secondary data sources. Primary data includes direct inputs from healthcare providers, whereas secondary data is gathered from wearable devices and questionnaires, tracking a range of configurable metrics such as physical activity, smoking habits, pain intensity and more. Although not all patients in the iHelp pilot studies are adhering to the data collection plans, it is established that the majority of patients would share their data with their HCP in long-term prevention activities.
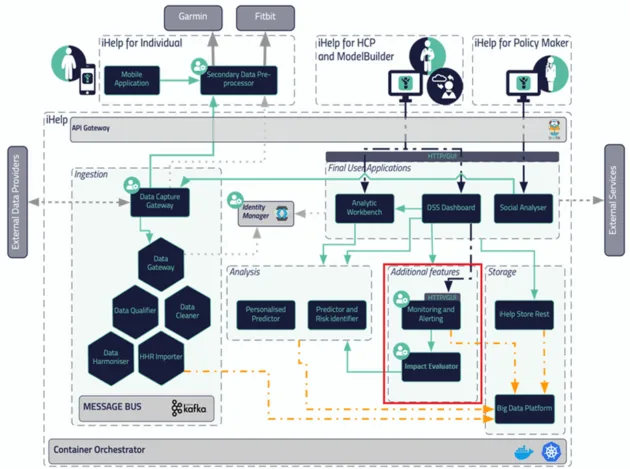
13 Figure 1 depicts the iHelp platform architecture and within it the Monitoring and Alerting component.
Figure 1. Overall iHelp Architecture, highlighting the two iHelp components of the MA&F subsystem, the Monitoring & Alerting and the Impact evaluator.
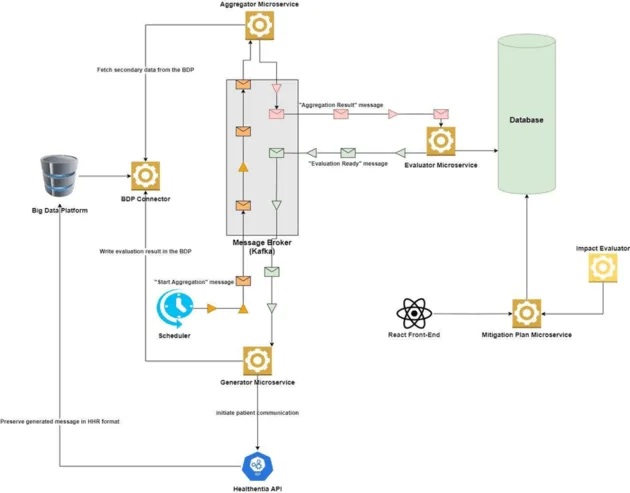
The mechanism has a two-fold objective, as it aims to optimize decision support for HCPs, while also offering improved personalization of risk mitigation and prevention plans through the fine-tuning of goal settings. To achieve the latter, four subcomponents are designed and developed, embodying a microservices architecture: the BDP Connector, the Data Aggregator, the Data Evaluator, and the Alert Generator that implement the monitoring, evaluating and alerting functionalities. These microservices are communicating through Apache Kafka,
14 a distributed event streaming platform that ensures high throughput, fault tolerance, and seamless scalability. Kafka enables the microservices to handle large volumes of data efficiently, making the system robust and adaptable to varying loads, which is essential for the dynamic environment of healthcare data processing. The latter is highly crucial especially in the case of exchanging (near) real-time streaming data. A respective performance evaluation during load testing showed the system can handle over 5000 messages per minute with latency below 100 ms per message under peak load.
The mechanism also provides a mitigation plans API for managing the CRUD (Create, Read, Update, Delete) operations related to the action plans and rules and their assignment to patients, controlling the lifecycle of action plans and rules tailored to individual patient needs. This microservice is integral to both the React-based frontend, providing a user-friendly interface for HCPs as part of the DSS, and the backend, where it interfaces with other microservices to ensure seamless operation and data flow. The BDP Connector acts as the bridge between the iHelp BDP and the internal workings of the monitoring system. Its primary role is to facilitate the secure and reliable extraction of patient data from the big data platform, making it available for further processing. This microservice is critical in the initial step of data collection, ensuring that comprehensive and up-to-date patient information is consistently fed into the system for analysis. Following data retrieval, the Data Aggregator microservice takes center stage. It is programmed to collect data related to each action plan and its rules at predetermined intervals from the BDP Connector. The aggregator systematically organizes this information, preparing it for detailed evaluation. This process involves compiling data relevant to individual patient health goals, setting the stage for a personalized analysis.
Next, the Data Evaluator microservice represents the analytical core of the system, where the aggregated data undergoes scrutiny against predefined rules tailored to each patient’s health objectives. This evaluation determines whether the patient’s activities and health metrics align with their targeted health outcomes, such as medication adherence or physical activity levels. Utilizing Kafka for real-time data processing, the Data Evaluator ensures that the analysis is both timely and reflective of the latest data, crucial for accurate health monitoring and intervention.
Upon completion of the evaluation, the Alert Generator microservice is responsible for the delivery of personalized feedback to patients through a dedicated API to Healthentia’s Smart Profiler that triggers the Virtual Coach. As a result, the Healthentia mobile app provides messages and dialogues aiming to convey the evaluation results in a personalized, understandable, and actionable manner, encouraging patients towards healthier behaviors and goal achievement and giving them further information on the benefits of healthy habits.
Additionally, the Data Generator microservice archives an overview of these communications within the big data platform, mapped into HHR, thereby enriching the patient’s longitudinal health record with valuable insights and interactions. Figure 2 depicts the internal workflow of the advanced monitoring mechanism.
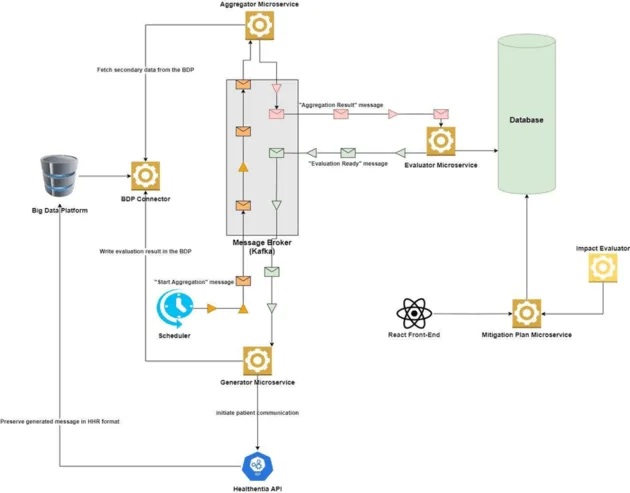
Figure 2. Monitoring and Alerting internal workflow.
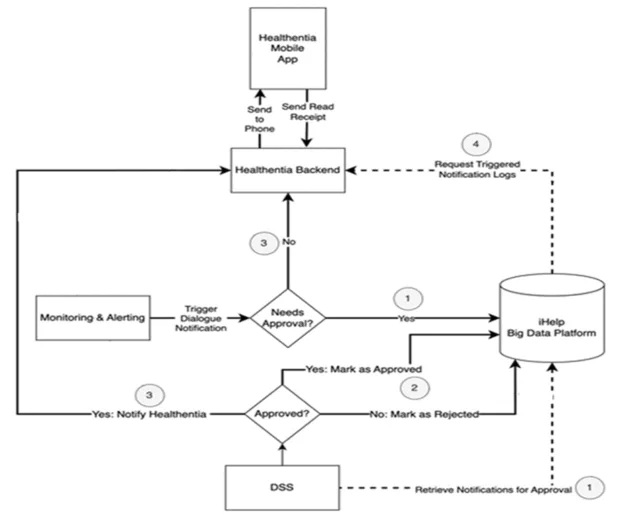
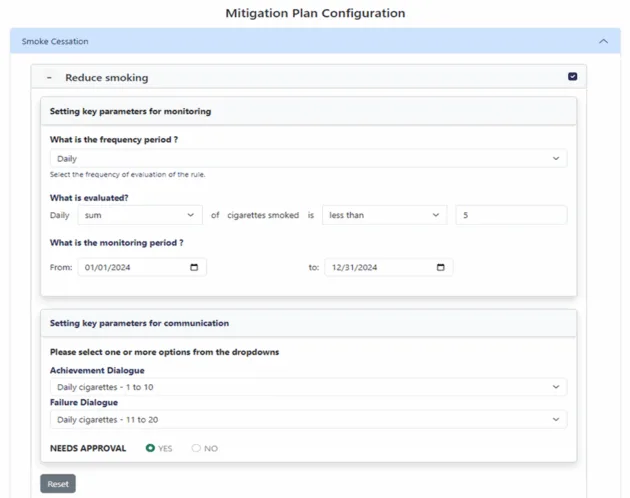
On the frontend side, the Monitoring and Alerting mechanism offers HCPs a React-based user interface (UI) to define offline rules and thresholds as part of the risk mitigation plans. The online evaluation of these rules in near real-time leads to dialogue proposals for the consideration of the HCPs, and the UI facilitates HCPs to make final selections for delivering the dialogues to patients. In that context, its main objective is to empower HCPs to assign mitigation plans and respective recommendations to a specific individual and then to monitor and assess the effect of these recommendations and plans in the lifestyle of the person. A mitigation plan is essentially an action plan assigned to a patient and typically the execution of this plan aims to bring concrete health improvements and to lower the risk of developing pancreatic cancer. It is comprised of several rules, some of which can be turned off, depending on the personalized configuration for the patient. The HCP will assign a goal value to each active rule of the mitigation plan selected for the patient. For example, a goal for a given patient can be to decrease the cigarettes smoked per day or to increase physical activity on a weekly basis. Then, the component will monitor and evaluate the progress of the patients by collecting and aggregating secondary (behavioral) data collected via the Healthentia mobile app, as self-reports or measurements, and then compare them with personalized targets issued by HCPs. To this end, Monitoring & Alerting enables the set of mitigation rules and facilitates the personalized interactions with the patients as depicted in Figure 3.
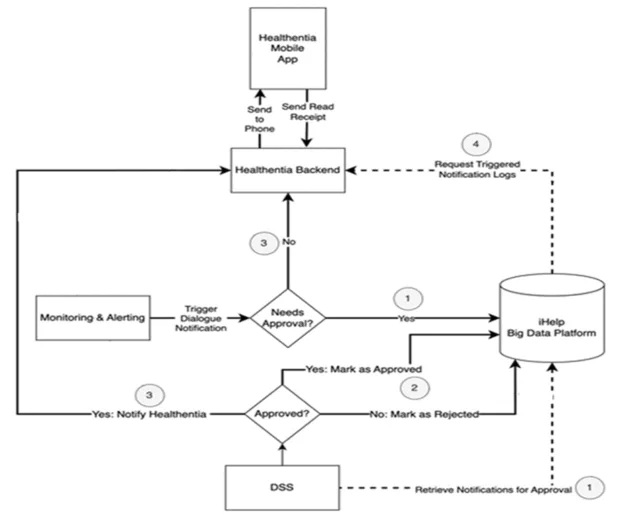
Figure 3. Inter-component communication.
The user journey begins when an HCP accesses the monitoring system’s UI through the DSS. This access point is the gateway to functionalities tailored to enhance patient care. It is also secured in compliance with the respective legal regulations towards an efficient access control and trustworthy data processing as described in Ref.
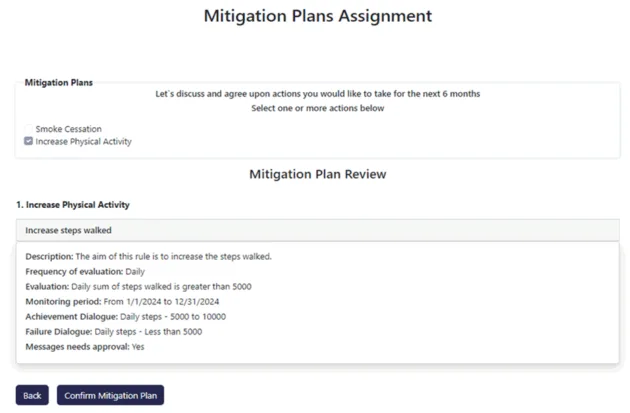
15. As shown in Figure 4, the HCP embarks on this process by assigning tailored mitigation plans and rules for each patient, which are crucial for guiding the patients towards healthier lifestyle choices and managing their health conditions effectively. After filling in all the settings, the HCP can see an overview of the assigned mitigation plan(s) for the current patient (Figure 5).
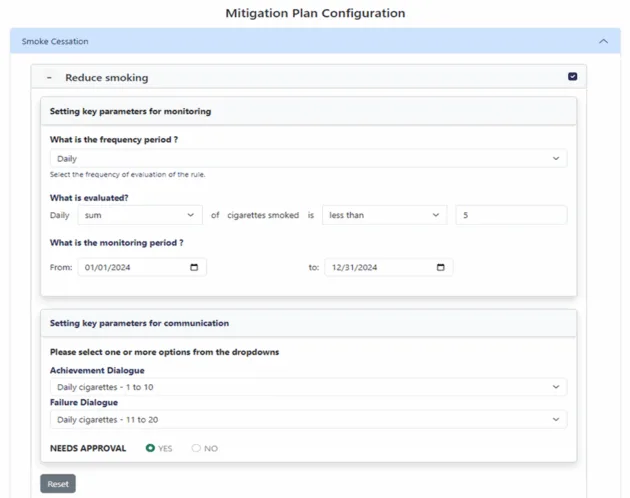
Figure 4. Configuration of mitigation plans.
Figure 5. Mitigation Plans Assignment in the advanced Monitoring and Alerting component.
Lowering or increasing one of the secondary data metrics is a feasible goal that can be assigned to a case. Such an example is the increase of the patient’s physical activity, by setting an attainable threshold (e.g., walking at least 10,000 steps a day), and trace it through physical data progress monitoring. Secondary data collection fluctuations of the past days/weeks, give information on the goal’s accomplishment or failure and drive possible re-evaluations from the health expert’s side or the machine learning algorithms of other components. The patients are informed of their progress or new assignments through the app dialogues served as push notifications to the Healthentia mobile app, and can also track their progress from the numerous widgets.
The iHelp platform supports two modes of communication of the outcomes derived from the evaluation of these rules: automatic communication of the evaluation results to the patient via the Healthentia API, or placing the outcomes in a pending state, requiring HCP’s approval before communication. This decision is pivotal as it dictates the subsequent flow of information and involves considerations of patient sensitivity, the gravity of the health information, and the need for personalized HCP intervention.
Following the initial setup, the monitoring system embarks on a continuous cycle of evaluation, operating in the background without the need for manual intervention. At every predefined interval, the system evaluates the patient’s data in relation to the assigned actions and rules. This automated process ensures timely assessment of the patient’s progress or adherence to personalized health goals.
If the HCP has opted for automatic communication, the system proceeds to inform the patient of their progress through the Healthentia API immediately after each evaluation cycle. This message or dialogue, encapsulating the outcome of the evaluation, is designed to be informative and motivational, fostering patient engagement with their health objectives. Furthermore, this continuous approach enables the iHelp platform to promote a way to enhance patient communication with an intelligent coaching element.
10 In contrast, if the HCP prefers to review the evaluation outcomes before the patient communication, the system stores an overview of the potential message in the BDP with a “proposed” status. This holding pattern allows for HCP oversight, ensuring that all patient communications are vetted for accuracy, appropriateness, and clinical relevance.
Concurrently, an overview of this communication is archived within the Big Data Platform (BDP) for record-keeping and future reference, ensuring a comprehensive health history is maintained.
The next phase involves HCP interaction with the DSS, where proposed communications are presented for review. The HCP accesses these messages through the DSS interface, where each message is accompanied by a “Send” button. This interface offers HCPs the flexibility to approve or reject the communication based on clinical judgment and patient-specific considerations.
Upon clicking “Send,” the approved message is dispatched to the patient via the Healthentia API, with its status in the BDP updated to “approved.” Conversely, if the HCP decides against sending the message, its status is updated to “rejected” in the BDP, and the message is withheld from patient communication. This step underscores the critical role of HCPs in curating and validating health information communicated to patients.
This overall workflow should be also supported by low response times that are essential for maintaining engagement, clinical utility, and the wider adoption of the system. Given the dynamic interaction model involving both automated and HCP-reviewed messaging workflows, any delays in patient feedback (either automatic or HCP-approved) could compromise timely intervention or behavior change momentum. Hence, the evaluation tests of the system were critical and it should be highlighted that they demonstrated an average response time of approximately 300 ms for HCP interface operations (e.g., assigning a mitigation plan, reviewing patient alerts, approving message dispatch). Moreover, the backend service availability exceeded 99.35% in high-demand simulations, supporting real-time communication with patients via the Healthentia API.
Virtual coach
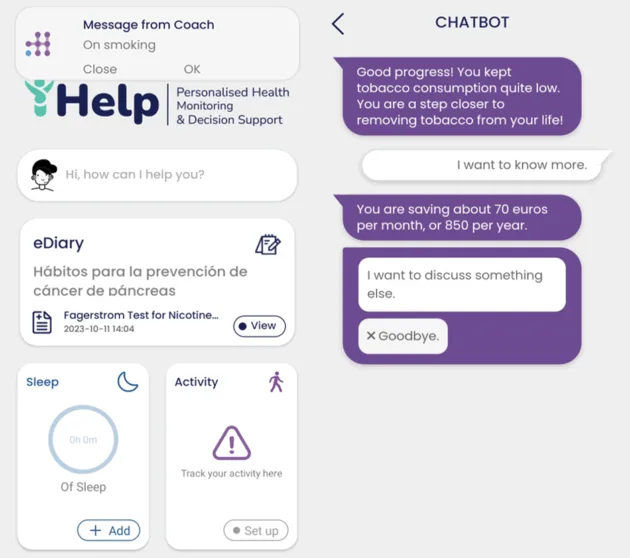
The Virtual Coach is a Healthentia component
9 that offers patients the UI for receiving and interacting with the delivered content at the mobile application. As such the component runs on the Healthentia mobile app, which is used as the iHelp patient companion app (facilitating data collection and advice delivery
10–12). Behind the scenes, it exposes an endpoint for receiving requests for dialogue delivery from the M&A component. In that call, the receiving patient and the intended dialogue are identified. Upon receiving the request, Healthentia pushes a notification to the mobile operating system (Android or iOS). The patient can tap either on the notification of the operating system, or on the notification at the dedicated application page. Then, the mobile view of the virtual coach is displayed, and the patient can go through the dialogue (Figure 6). After dialogue playback, the patient can still see the notification in the dedicated page, along with a summary of what it was about as a reference. The dialogues are handled (authored and played back) in the virtual coach using the open-source WOOL platform.
16
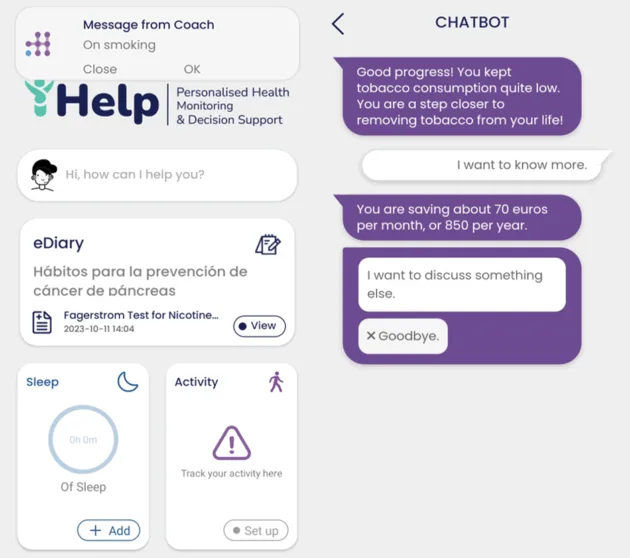
Figure 6. Handling dialogues at the Healthentia mobile app. A notification is sent to the patient (left), which leads to the dialogue playback UI (right).
The dialogue selection procedure depends on the nature of the message to be delivered, and can be carried out both by the iHelp system (health experts and ML models) or Healthentia’s decision making smart component – the Smart Profiler,17 detailed below. Both components leverage the patterns of the newly collected secondary data and perform evaluations on thresholds and goal achievements. The Monitoring and Alerting (M&A) component is responsible for triggering communications on achievements/failures of mitigation plans and introducing new actions to the end users. The dialogue content is triggered when the M&A rules indicate so. The Smart Profiler is responsible for choosing and triggering educational content, that appears to the users as tips on coping with the disease, the importance of their assigned actions, and the ways of achieving their goals adopting a healthier lifestyle. The educational content is also delivered in dialogues, daily selected by the Smart Profiler.
Smart profiler
The Smart Profiler is the intelligent system that makes decisions on advice delivery inside Healthentia.
17 It decides which educational dialogue should be triggered for a given user, based on the user’s data. The Smart Profiler is an expert system, evaluating rules associated with each educational item. These rules allow enumerating the importance of each item, based on the user data at the given time. Each rule is represented in the database as a mathematical expression (see example below) and is associated with one or more dialogues.
Dialogue selection starts with the evaluation of all the rules associated with the candidate dialogues, returning the initial playback probability of each dialogue. These initial probabilities are further weighted based on frequency of dialogue repetition and on dialogue impact. The probability of a dialogue selected frequently in the recent past is penalized for the future, to avoid the repetition of the same content for the same user, and thus make the dialogues more interesting and engaging. Impact is calculated through evaluating the short-term effect of the dialogue. If the. This is calculated as the ratio of the probability evaluation at the time of selection, and the average probability in the coming 3 days. If the probabilities in at least short-term are reduced, then the Smart Profiler decides the dialogue has a positive impact. The initial probabilities are weighted by that ratio calculated the previous time the dialogue was played back, increasing them for impactful dialogues.
Besides rule evaluation, the Smart Profiler also considers the optimal time within the day for sending a notification to the user, based on app usage logging. The system maintains a histogram of interactions with the mobile app versus time of day. Given a time interval, the histogram yields the optimum time for the next communication. This feature ensures that the notification will reach the end-user at the most optimal time, for them to pay attention and interact with the app and the coach. Figure 7 shows the conceptual architecture of content delivery decisions and triggers in iHelp. Decisions and recommendations are made either internally by the Smart Profiler, or externally by the iHelp M&A, and the dialogue ID selected for triggering is eventually passed to the VC service, responsible to make the request for serving the content. The serving itself is managed via WOOL.
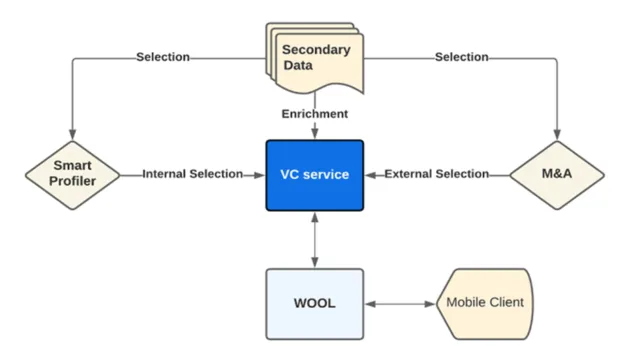
Figure 7. Internal and external decision making and triggering of a feedback dialogue for the Alerting component.
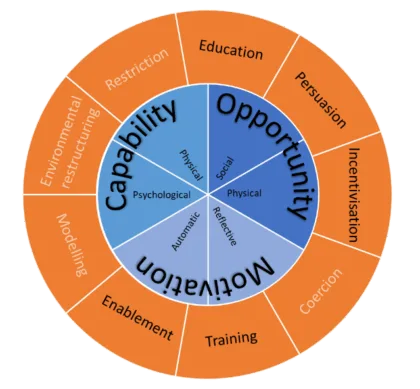
The mechanism described in Figure 7 works towards achieving changes in the lifestyle of patients. These changes are interrelated with better self-management when dealing with chronic diseases. Factors ranging from education and understanding of the principles of a condition to limiting behavioral risk factors in different domains of behavior enable a defense against multi-sided chronic illnesses effects: comorbidities, diminished mental health and exacerbations. The Smart Profiler focuses on six domains: Physical activity, sleep, nutrition, self-care, smoking cessation and emotional health. Healthentia’s dialogues delivered by the Virtual Coach address factors and habits that may lead to risk behaviors, aiming at extended lifespan and health span of patients. Successful interventions for life-changing actions must be underpinned by theoretically-driven behavior change models for long lasting results,
18 the Smart Profiler implements the Behavior Change Wheel (BCW) intervention design by Michie et al., for delivering life changing content and advice.
19 Out of the various frameworks designed to serve and drive behavioral change,
20 BCW is an incorporation of 19 frameworks into a single coherent tool (Figure 8). The tool assesses the patient’s capability (C), opportunity (O), and motivation (M) for behavior (B) change (the COM-B model
21). The behavioral change framework implemented within the Smart Profiler works along these three sources of human behavior, capability, opportunity and motivation, considering five intervention functions, namely Education, Training, Persuasion, Enablement and Incentivisation (out of the out of the nine functions introduced by the BCW). Different techniques can be applied for each intervention function, and Healthentia’s dialogues are assigned to these techniques. The Smart Profiler uses each patient’s contextual profile, including behavioral trends, current health goals, historical responses to dialogue types, and wearable/self-report data, to prioritize which intervention function (e.g., Persuasion vs Enablement) should be emphasized ensuring personalized behavioral alignment. For instance, a patient struggling with adherence might receive more persuasive and incentivizing dialogues, while one already engaged may receive educational reinforcement. This adaptive logic ensures that each dialogue delivered is behaviorally aligned and clinically relevant. The Smart Profiler ranks the domains, intervention functions and finally techniques, effectively selecting dialogues.
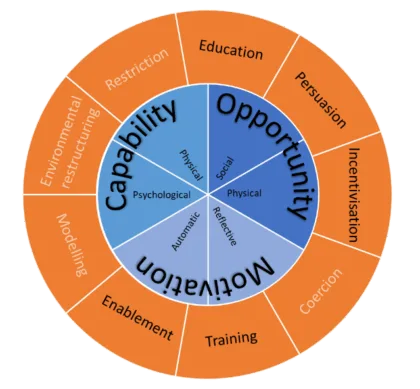
Figure 8. The Behavioral Change Wheel: The inner disk features the three sources of behavior, while the outer ring depicts the nine intervention functions, of which only the five in black are implemented within the Smart Profiler.
Discussion
The personalized dialogue and coaching system is an impactful innovation of the iHelp platform. It breaks the communication barriers between healthcare providers and receivers and facilitates behavioral change in patients and citizens by empowering them to understand their condition and providing easy to understand directions on how to manage their health. The rule-based dialogue selection system implemented in the Monitoring and Alerting mechanism effectively delivers personalized education and advice, thus impacting the everyday life of the patient or citizen at risk of developing cancer. Improved emphasis and understanding of the behavioral data can lead to improvements on the clinical condition of the patient, and change their lives for the better, as reported by the end-users of the solutions during the impact assessment performance. However, it is important to note that the questionnaires used to gather impact data were adapted from existing tools and pilot-tested but not formally validated for this specific study. To this end, there is the need to highlight that while the preliminary insights remain valuable, further validation in real-world setting and other use cases is envisioned to ensure the robustness and generalizability of the findings. Another limitation of this research work is that a thorough assessment of system usability, especially in the context of the HCP interface and patient-facing mobile app, was not feasible within the project’s timeline and this important dimension will be considered for inclusion in future work and projects.
Impact evaluator
The Impact Evaluator is responsible for evaluating the impact of the advice sent to groups of citizens/patients, as this advice is carried out via dialogues related to mitigation plans stemming from risk factors. It is shown in the overall iHelp architecture in Figure 1. The main goal is to monitor the behavior of citizens/patients and highlight to the HCPs how and if the specific type of advice changed the lifestyle of the recipients. For doing that, the citizens/patients are clustered using common characteristics (e.g. age, gender, BMI, or risk factors, if available) to compare the advice sent to a similar population). The result of this analysis should contribute to better finetune the model for generating the advice and the user to be reached. The input data is collected on demand of the HCP, both from the Monitoring and Alerting component (the goals, thresholds and their achievement) and the collected data (from the HHR using the standard FHIR API
8). The impact is then evaluated, and the result is shown to the HCP through the dedicated iHelp platform interface.
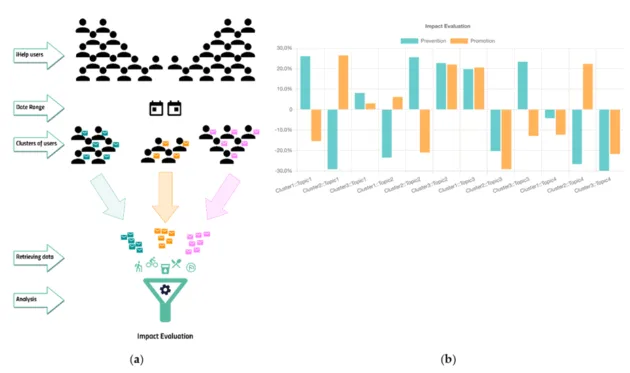
The process is depicted in Figure 9. After clustering the advice recipients, the Impact Evaluator highlighted that for Topic1, a Cluster1 of people had a positive and healthy behavior after they received some prevention-based messages, but that was not the case for the promotion-based messages. Completely the opposite behavior was observed in Cluster2. Cluster3 of Topic1 remained unaffected. The percentage represented on the ordinate axis is the delta percentage of the achieved goal between the period before and after receiving the messages.
Figure 9. Clustering and Results. (a) Depicts the user journey and clustering approach of the Impact Evaluator; (b) Showcases an initial example of the final outcome.
Results
iHelp was evaluated during pilot studies that focused on the applicability of the clinical and technical outcomes through representative scenarios, while providing useful feedback about the iHelp concepts and technologies. Five pilot studies, carried out during the progress of the project, aimed to address three different aspects of the management of cancer: Primary prevention, Secondary prevention and Monitoring of treatments, while widening the field of types of cancers tackled to four, namely prostate, breast, anal and liver cancer. All pilots and technical partners worked in performing impact assessments (qualitative and quantitative) on both technological implementations and social factors, in the scope of prevention, early detection and treatment of cancer.
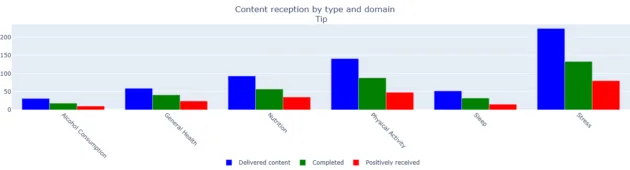
In all three cases the MA&F subsystem of iHelp delivered content to the patients. In total 600 items of content have been delivered. These span six domains: alcohol consumption (5.17% of the total content), general health including smoking cessation (9.83%), nutrition (15.5%), physical activity (23.5%), sleep (8.67%) and stress (37.3%). The patient then has the option to ignore or go through the content (complete it). Then they can choose to offer feedback on completed content. Some of it is positive. The volume of delivered, completed and positively received content across the different domains is shown in Figure 10.
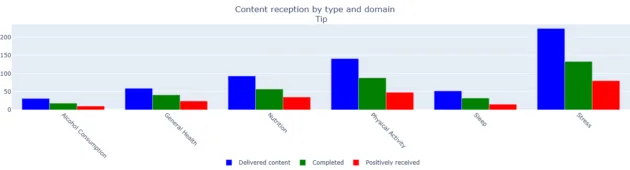
Figure 10. Volume of delivered, completed and positively received content across the six domains.
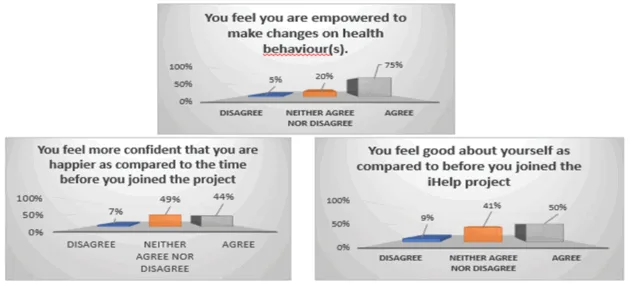
While technological assessment is of high priority for any component made and destined to serve clinical studies, health experts and patients, the assessment of the impact of iHelp outcomes on socio-physical, mental and societal factors positively influencing a person’s health and life, remains the ultimate challenge. The evaluation of the program involved reports (questionnaires) to both clinicians participating in the study and end-users of the solution offered, on four main domains: physical, psychosocial, health knowledge and social aspects. Questionnaires were distributed online or on hospital premises after a specific timeframe of enrolment into the study or upon study completion, and the results are shown in Figure 11. It should be noted that these questionnaires were created and adapted based on existing instruments but were not validated for this specific study. They were, however, pilot-tested before deployment.
Figure 11. Evaluation of the iHelp solution impacts on patients’ lives.
Discussion
The personalized dialogue and coaching system is an impactful innovation of the iHelp platform. It breaks the communication barriers between healthcare providers and receivers and facilitates behavioral change in patients and citizens by empowering them to understand their condition and providing easy to understand directions on how to manage their health. The rule-based dialogue selection system implemented in the Monitoring and Alerting mechanism effectively delivers personalized education and advice, thus impacting the everyday life of the patient or citizen at risk of developing cancer. Improved emphasis and understanding of the behavioral data can lead to improvements on the clinical condition of the patient, and change their lives for the better, as reported by the end-users of the solutions during the impact assessment performance. However, it is important to note that the questionnaires used to gather impact data were adapted from existing tools and pilot-tested but not formally validated for this specific study. To this end, there is the need to highlight that while the preliminary insights remain valuable, further validation in real-world setting and other use cases is envisioned to ensure the robustness and generalizability of the findings. Another limitation of this research work is that a thorough assessment of system usability, especially in the context of the HCP interface and patient-facing mobile app, was not feasible within the project’s timeline and this important dimension will be considered for inclusion in future work and projects.
Conclusions
This research work introduced the conceptual design and prototype development of a novel patient monitoring system applied on advancing the early risk mitigation of pancreatic cancer. The prototype integrates a core Monitoring and Alerting component, supported by several sub-components and microservices based on a modular architecture. This design ensures interoperability and demonstrates the system’s ability to integrate with divergent mechanisms and components and a seamless deployment into real-world settings and environments. The latter is facilitated through the utilisation of clinical, behavioral, and patient-reported data, enabling HCPs to design and assign tailored mitigation plans, while supporting patients through adaptive coaching and continuous feedback.
Initial pilot evaluations presented in this manuscript highlighting the feasibility of the system in real-world healthcare environments. The qualitative and quantitative analysis of the results suggest that the platform can effectively deliver actionable insights and promote adoption of healthier behaviors by the individuals following personalized mitigation plans designed by their HCPs. Moreover, the clustering-based Impact Evaluator offers an evidence-driven approach to understanding how tailored feedback influences patient subgroups, thereby informing future refinements.
These achievements highlight the importance of designing and deploying scalable and patient-centered solutions in the modern healthcare landscape that also focus on integrating predictive analytics with personalized interventions and recommendations. This will further result to a more preventive, participatory, and data-driven model of care as HCPs will be empowered with advanced monitoring tools and patients will be engaged into a better management of their own health.
Acknowledgments
The authors wish to acknowledge the contribution of all the technical and medical partners of the iHelp consortium in setting up the iHelp platform and conducting the pilot studies.
Ethical considerations
This research was conducted under the scopes of the iHelp project. The pilot studies were conducted according to the guidelines of the Declaration of Helsinki and approved by the Research Ethics Committee of the Marina Salud S.A. (Ref: C.P. iHelp, C.I. 22/531-E; 3 October 2022), the Fondazione Policlinico Universitario Agostino Gemelli IRCCS – Comitato Etico, ID 4820, approval: 23/06/2022, amendment approval: 19/01/2023, the Medical University of Plovdiv Science Ethics Committee Protocol № 7/13.10.2022, Reg. № P 2504/11.11.2022, and the University Research Ethics Committee 3, Ref: 2022-13644-23283, approval date 09/05/2022. Written informed consent has been obtained from all subjects participated in these studies.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the European Union’s project iHelp, grant number 101017441. This work has been partly supported by the University of Piraeus Research Center.
References
1. Paschou M and Sakkopoulos E. Personalized assistant apps in healthcare: a systematic review. In: Proceedings of the 2019 10th International Conference on Information, Intelligence, Systems and Applications (IISA), PATRAS, Greece, July 2019. IEEE, pp. 1–8.
2. Anthonia Okolo C, Babawarun O, Arowoogun JO, et al. Rawlings chidi the role of Mobile health applications in improving patient engagement and health outcomes: a critical review. Int J Sci Res Arch 2024; 11: 2566–2574.
3. Dhar E, Bah AN, Chicchi Giglioli IA, et al. A scoping review and a taxonomy to assess the impact of Mobile apps on cancer care management. Cancers 2023; 15: 1775.
4. Manias G, Op Den Akker H, Azqueta A, et al. iHELP: personalised health monitoring and decision support based on artificial intelligence and holistic health records. In: Proceedings of the 2021 IEEE Symposium on Computers and Communications (ISCC). Athens, Greece, September 5 2021: IEEE, pp. 1–8.
5. Manias G, Azqueta-Alz´uaz A, Damiani A, et al. An enhanced standardization and qualification mechanism for heterogeneous healthcare data. In: H¨agglund M, Blusi M, Bonacina S, et al. (eds). Studies in Health Technology and Informatics. IOS Press, 2023. ISBN 978-1-64368-388-1.
6. Manias G, Kouremenou E, Alz´uaz AA, et al. An optimized pipeline for the processing of healthcare data towards the creation of holistic health records. In: Proceedings of the 2023 International Conference on Applied Mathematics & Computer Science (ICAMCS), Lefkada Island, Greece, August 8 2023. IEEE, pp. 50–56.
7. Ke TM, Lophatananon A and Muir KR. Risk factors associated with pancreatic cancer in the UK bioban cohort. Cancers 2022; 14: 4991.
8. Manias G, Azqueta-Alz´uaz A, Dalianis A, et al. Advanced data processing of pancreatic cancer data integrating ontologies and machine learning techniques to create holistic health records. Sensors 2024; 24: 1739.
9. Op Den Akker H, Cabrita M and Pnevmatikakis A. Digital therapeutics: virtual coaching powered by artificial intelligence on real-world data. Front Comput Sci 2021; 3: 750428.
10. Kyriazakos S, Pnevmatikakis A, Cesario A, et al. Discovering composite lifestyle biomarkers with artificial intelligence from clinical studies to enable smart eHealth and digital therapeutic services. Front Digit Health 2021; 3: 648190.
11. Pnevmatikakis A, Kanavos S, Matikas G, et al. Risk assessment for personalized health insurance based on real-world data. Risks 2021; 9: 46.
12. Kyriazakos S, Pnevmatikakis A, Op Den Akker H, et al. The role of big data and artificial intelligence in clinical research and digital therapeutics. In: Cesario A, D’Oria M, Auffray C, et al. (eds). Personalized Medicine Meets Artificial Intelligence. Springer International Publishing, 2023, pp. 63–81. ISBN 978-3-031-32613-4.
13. Bove LA. Increasing patient engagement through the use of wearable technology. J Nurse Pract 2019; 15:535–539.
14. Narkhede N. Kafka: the definitive guide: real-time data and stream processing at scale. 1st ed. O’Reilly Media, 2016. ISBN 978-1-4919-3616-0.
15. Chen Y, Sun W, Zhang N, et al. Towards efficient fine-grained access control and trustworthy data processing for remote monitoring services in IoT. IEEE Trans Inf Forensics Secur 2019; 14: 1830–1842.
16. Beinema T, Op Den Akker H, Hofs D, et al. The WOOL dialogue platform: enabling interdisciplinary userfriendly development of dialogue for conversational agents. Open Res Europe 2022; 2: 7.
17. Beinema T, Op Den Akker H, Hermens HJ, et al. What to discuss? A blueprint topic model for health coaching dialogues with conversational agents. Int J Hum Comput Interact 2023; 39: 164–182.
18. Michie S and Abraham C. Interventions to change health behaviours: evidence-based or evidenceinspired? Psychol Health 2004; 19: 29–49.
19. Michie S, Van StralenMMandWest R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011; 6: 42.
20. Ara´ujo-Soares V, Hankonen N, Presseau J, et al. Developing behavior change interventions for selfmanagement in chronic illness: an integrative overview. Eur Psychol 2019; 24: 7–25.
21. Barker F, Atkins L and De Lusignan S. Applying the COM-B behaviour model and behaviour change wheel to develop an intervention to improve hearing-aid use in adult auditory rehabilitation. Int J Audiol 2016; 55: S90–S98.
Keywords: personalized healthcare, remote patient monitoring, behavioral change
More Publications